(Editor’s note: The content on BarBend is meant to be informative in nature, but it shouldn’t take the place of advice and/or supervision from a medical professional. The opinions and articles on this site are not intended for use as diagnosis, prevention, and/or treatment of health problems. If you’re dealing with or exhibiting signs of depression, please seek the advice of a medical professional immediately.)
A very big, very high quality meta analysis is drawing interesting connections between how you eat and how you feel. The research, published this month in Psychosomatic Medicine, looked at sixteen randomized controlled trials, which are considered extremely high quality as far as studies go. Over 45,000 people were included in the research.(1)
The meta-analysis concluded that food quality exerts a significant effect on depression among non-clinically depressed populations. The interventions varied but nine studies focused on improving nutrient intake, with the others emphasizing lower fat intake and reducing body weight.
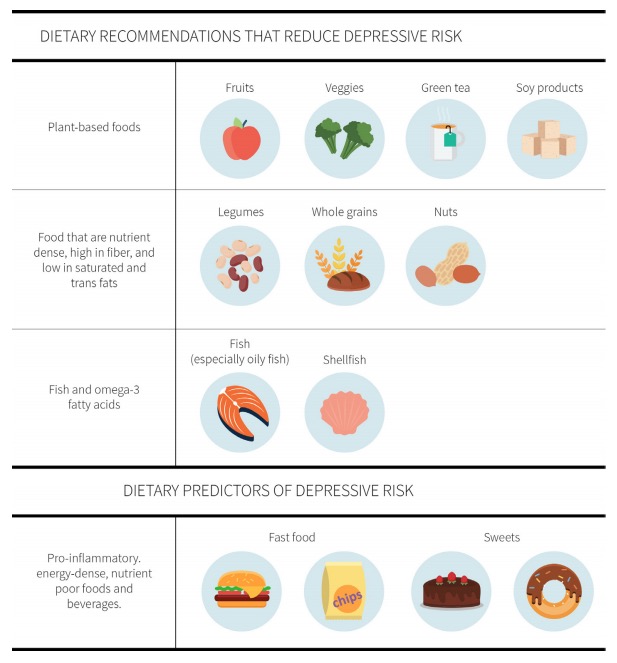
So what does improving nutrient intake mean? This isn’t one of those studies that has a neat conclusion like “blueberries reduce depression” or “spinach helps with anxiety” — the interventions had broader foci but they generally emphasized high-fiber, micronutrient-dense fruits and vegetables, and minimized processed foods that are high in fat and sugar.
The findings reflect other research that has correlated a reduction in depressive symptoms with more fiber, plant-based whole foods, and fatty fish.(2)(3)(4) It’s also important to emphasize that whole foods, in particular those that are plant-based, aren’t just sources of vitamins and minerals but also phytochemicals and antioxidants, which have also been linked to lower levels of depression — possibly in part due to their beneficial impact on inflammation.(5)
[Learn more: The Best Omega-3 Supplements for Fighting Inflammation.]
Image courtesy of the Examine.com Research Digest’s analysis of this study.
There are many pathways that might affect depression, including oxidative stress, inflammation, gut health, and body weight. A wide variety of foods that deliver plenty of nutrients and fiber is key to managing these factors and lowering the risk. (It’s also more cost effective than other methods, though we’re not implying that other methods are less effective.)
[Learn more about the possible connection between probiotic bacteria and mental health.]
The findings are important because depression affects over 300 million people worldwide, and the number of people affected increased by almost 20 percent between 2005 and 2015. These numbers don’t even account for sub-clinical symptoms that can still negatively affect quality of life. Given the cost of healthcare and decreased productivity, better understandings of lifestyle treatments could have a profound impact on the economy in addition to the more obvious potential benefits on the individuals themselves.
Note that while food quality does have a significant effect, the research didn’t find diet was more significant than psychotherapy or drugs, so it doesn’t seem to be smart to try and self medicate without the intervention of a medical expert. Be sure to speak with a mental health practitioner if you’re dealing with or exhibiting any signs of depression — you can find one near you here.
References
1. Firth J, et al. The Effects of Dietary Improvement on Symptoms of Depression and Anxiety: A Meta-Analysis of Randomized Controlled Trials. Psychosom Med. 2019 Apr;81(3):265-280.
2. Miki T, et al. Dietary fiber intake and depressive symptoms in Japanese employees: The Furukawa Nutrition and Health Study.Nutrition. 2016 May;32(5):584-9.
3. Liu X, et al. Fruit and vegetable consumption and the risk of depression: A meta-analysis. Nutrition. 2016 Mar;32(3):296-302.
4. Grosso G, et al. Omega-3 fatty acids and depression: scientific evidence and biological mechanisms. Oxid Med Cell Longev. 2014;2014:313570.
5. Sureda A, et al. Polyphenols and depression: from chemistry to medicine.Curr Pharm Biotechnol. 2015;16(3):259-64.